From Mouth to Gut: Connective Pathways between Oral Health and Digestive Disorders
Let’s face it: most of us don’t give much thought to the connection between our mouth and our gut. Sure, we know that what we eat affects our digestion, but did you know that the health of your mouth can actually influence your digestive system in ways you might not expect? It’s true—your oral health and gut health are more intertwined than you might think.
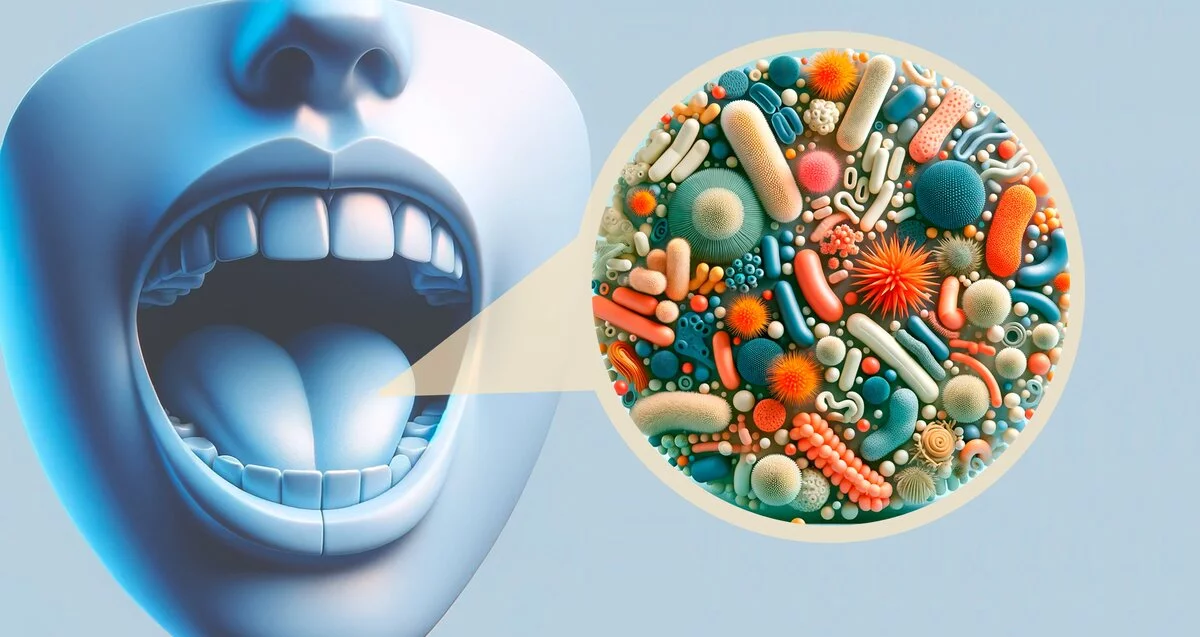
Think of your mouth as the front door to your body. Everything you eat and drink passes through it, but so do bacteria, pathogens, and other microscopic troublemakers. When your oral health is in tip-top shape, it acts like a bouncer, keeping the bad stuff out. But when it’s not? Well, let’s just say those troublemakers can sneak in and cause chaos all the way down to your gut.
In this article, we’re diving deep into the fascinating connection between oral health and digestive disorders. We’ll explore how bacteria from your mouth can travel to your gut, why good oral hygiene is a game-changer for preventing digestive issues, and even uncover the concept of “leaky mouth” (yes, it’s a thing). By the end, you’ll have a whole new appreciation for your toothbrush—and maybe even your floss.
So, grab a cup of coffee (or tea, if that’s your jam) and let’s get into it. Your mouth—and your gut—will thank you.
How Pathogens Travel from Mouth to Gut
You might not think twice about the bacteria in your mouth, but here’s something to chew on: your oral health has a direct line to your gut. Yep, your mouth isn’t just the gateway to your favorite foods—it’s also a VIP entrance for bacteria and pathogens that can wreak havoc on your digestive system.
So, how does this happen? Every time you swallow, you’re not just sending down that bite of pizza or sip of coffee. You’re also transporting saliva, which carries millions of bacteria—both good and bad—straight into your gastrointestinal tract. While some bacteria are harmless (or even helpful), others can throw your gut microbiome out of whack.
Take Helicobacter pylori (H. pylori), for example. This pesky bacterium is a common culprit behind stomach ulcers and even some cases of gastritis. And guess where it often starts its journey? Yep, your mouth. Poor oral hygiene can create a breeding ground for H. pylori, allowing it to hitch a ride to your stomach and cause trouble.
But it’s not just H. pylori. Other harmful bacteria, like those linked to gum disease, can also make their way down to your gut. Once there, they can contribute to inflammation, disrupt your gut’s natural balance, and even play a role in conditions like irritable bowel syndrome (IBS) or acid reflux.
Think of it like this: your mouth is the front door to your digestive system. If you leave that door wide open for harmful bacteria, don’t be surprised if they wander in and throw a party in your gut. The good news? You’ve got the power to lock that door—or at least keep it guarded—with some simple, consistent oral hygiene habits.
So, next time you’re brushing your teeth, remember: you’re not just protecting your pearly whites. You’re also safeguarding your gut. And trust me, your stomach will thank you later.
The Role of Oral Hygiene in Preventing Digestive Disorders
Let’s get real for a second: brushing and flossing might feel like just another chore on your to-do list, but they’re way more important than you think. Good oral hygiene isn’t just about avoiding cavities or keeping your breath fresh—it’s a key player in keeping your digestive system running smoothly.
Here’s the deal: when you neglect your oral health, harmful bacteria can build up in your mouth, leading to issues like gum disease (aka periodontal disease). And gum disease isn’t just bad news for your teeth—it can send those nasty bacteria straight to your gut, where they can cause all sorts of trouble.
For instance, studies have shown a link between gum disease and conditions like irritable bowel syndrome (IBS), stomach ulcers, and even acid reflux. How? Well, when your gums are inflamed, they become a hotspot for bacteria to thrive. These bacteria can then travel down your digestive tract, disrupting the delicate balance of your gut microbiome.
Think of your gut microbiome as a bustling city. When everything’s in harmony, it’s a well-oiled machine. But when harmful bacteria crash the party, it’s like a traffic jam in the middle of rush hour—nothing works the way it should. This imbalance can lead to bloating, cramping, and other digestive discomforts that no one wants to deal with.
The good news? You can keep these troublemakers in check with some simple habits:
- Brush twice a day: Use a fluoride toothpaste to keep bacteria at bay.
- Floss daily: Get rid of food particles and plaque hiding between your teeth.
- Visit your dentist regularly: Professional cleanings can remove stubborn buildup you can’t tackle at home.
By taking care of your mouth, you’re not just protecting your smile—you’re also giving your gut a fighting chance. So, the next time you’re tempted to skip flossing, remember: your gut is counting on you. And hey, who doesn’t want to feel good from mouth to gut?
The Concept of “Leaky Mouth” and Its Impact on Digestion
You’ve probably heard of “leaky gut,” but have you ever heard of “leaky mouth”? No, it’s not some weird new trend—it’s a real concept that could explain why your oral health and digestive system are more connected than you think.
So, what exactly is “leaky mouth”? Think of it like this: your mouth is lined with a protective barrier, much like your gut. When this barrier is healthy, it keeps harmful bacteria and toxins from entering your bloodstream. But when it’s compromised—say, from gum disease, untreated cavities, or chronic inflammation—it becomes “leaky,” allowing bacteria and toxins to slip through and wreak havoc elsewhere in your body, including your gut.
This isn’t just a theory. Research suggests that oral bacteria entering the bloodstream can trigger systemic inflammation, which can then affect your digestive system. For example, studies have found that people with gum disease are more likely to experience conditions like Crohn’s disease, ulcerative colitis, and even acid reflux.
Here’s how it works: when harmful bacteria from your mouth enter your bloodstream, they can travel to your gut and disrupt the delicate balance of your microbiome. This disruption can lead to inflammation, which is a key player in many digestive disorders. It’s like a domino effect—one small problem in your mouth can set off a chain reaction that impacts your entire digestive system.
But don’t panic just yet. The good news is that you can take steps to prevent “leaky mouth” and protect your gut:
- Treat oral infections promptly: Don’t ignore cavities, gum disease, or other oral health issues.
- Stay hydrated: A dry mouth is a breeding ground for bacteria, so drink plenty of water.
- Eat a balanced diet: Foods rich in vitamins and minerals can strengthen your oral and gut health.
By keeping your mouth healthy, you’re not just protecting your teeth and gums—you’re also building a strong defense for your gut. So, the next time you hear someone say, “It all starts in the mouth,” you’ll know they’re not just talking about chewing. Your mouth and gut are teammates, and when one’s in trouble, the other feels it too. Let’s keep both in tip-top shape, shall we?
Actionable Strategies for Prevention
Alright, let’s get down to brass tacks. You now know how closely your oral health and digestive system are linked, but what can you actually do about it? The good news is, you don’t need a PhD in biology or a fancy medical degree to protect both your mouth and your gut. With a few simple, actionable strategies, you can keep both systems running like a well-oiled machine.
1. Step Up Your Oral Hygiene Game
This one’s a no-brainer, but it’s worth repeating. Your daily oral care routine is your first line of defense against harmful bacteria. Here’s how to do it right:
- Brush twice a day: Use a fluoride toothpaste and spend at least two minutes brushing. Don’t forget to gently brush your tongue—it’s a hotspot for bacteria.
- Floss daily: Flossing removes plaque and food particles from places your toothbrush can’t reach. If traditional floss feels like a hassle, try floss picks or a water flosser.
- Rinse with mouthwash: An antimicrobial mouthwash can help kill bacteria and freshen your breath. Just don’t use it as a substitute for brushing and flossing!
2. Schedule Regular Dental Check-Ups
Even if you’re a brushing and flossing pro, you still need to see your dentist regularly. Professional cleanings remove stubborn plaque and tartar that you can’t tackle at home, and your dentist can catch potential issues (like cavities or gum disease) before they become big problems. Aim for a check-up every six months—or more often if your dentist recommends it.
3. Fuel Your Body with Gut-Friendly Foods
What you eat doesn’t just affect your waistline—it impacts your oral and gut health too. Here are some foods that can help keep both systems happy:
- Probiotics: Yogurt, kefir, sauerkraut, and other fermented foods introduce good bacteria to your gut.
- Fiber-rich foods: Fruits, vegetables, and whole grains promote healthy digestion and can even help scrub your teeth clean.
- Crunchy foods: Apples, carrots, and celery act like natural toothbrushes, stimulating saliva production and scrubbing away plaque.
4. Stay Hydrated
A dry mouth is a playground for bacteria. Drinking plenty of water throughout the day helps wash away food particles and bacteria, keeping your mouth and gut in better shape. Plus, water is essential for digestion, so it’s a win-win.
5. Kick Bad Habits to the Curb
Smoking and excessive alcohol consumption aren’t just bad for your overall health—they’re terrible for your mouth and gut too. Smoking increases your risk of gum disease, while alcohol can dry out your mouth and disrupt your gut microbiome. If you need help quitting, talk to your doctor or dentist.
6. Listen to Your Body
If something feels off—whether it’s persistent bad breath, bleeding gums, or digestive discomfort—don’t ignore it. These could be signs that your oral or gut health needs attention. The sooner you address the issue, the better.
By taking these steps, you’re not just protecting your smile—you’re investing in your overall health. Remember, your mouth and gut are teammates, and when one thrives, the other does too. So, let’s give them both the care they deserve. Your future self will thank you!
Conclusion
When it comes to your health, everything is connected—and your mouth and gut are no exception. From the way harmful bacteria travel from your mouth to your gut to the concept of “leaky mouth” and its impact on digestion, it’s clear that oral health plays a starring role in your overall well-being.
By understanding this mouth-gut connection, you’re already one step ahead. But knowledge alone isn’t enough—it’s what you do with it that counts. Whether it’s stepping up your oral hygiene routine, eating gut-friendly foods, or scheduling regular dental check-ups, every small action adds up to big benefits for both your mouth and your digestive system.
So, what are you waiting for? Your mouth and gut are counting on you to take charge of their health. Start today by booking that dental appointment, swapping out sugary snacks for crunchy veggies, or simply committing to floss every night. Your body will thank you—and who knows? You might just feel better from head to toe.
Ready to take the next step? Call your dentist or healthcare provider to discuss how you can optimize your oral and digestive health. After all, when it comes to your well-being, every little bit helps. Let’s keep that smile—and your gut—happy and healthy!
FAQs
Q: How are oral health and the digestive system connected?
A: The mouth is the entry point to the digestive system. Oral bacteria and inflammation can travel to the gut, impacting its health and function.
Q: Can poor oral hygiene contribute to digestive problems?
A: Yes. Poor oral hygiene can lead to an overgrowth of harmful bacteria that, when swallowed, can disrupt the gut microbiome and potentially trigger or worsen digestive disorders.
Q: What specific oral health issues are linked to digestive disorders?
A: Periodontal (gum) disease, tooth decay, and oral infections have been linked to an increased risk or severity of conditions like inflammatory bowel disease (IBD) and acid reflux.
Q: Can digestive disorders affect oral health?
A: Absolutely. Conditions like Crohn’s disease, ulcerative colitis, and GERD can manifest with oral symptoms such as ulcers, dry mouth, altered taste, and enamel erosion.
Q: How does the gut microbiome relate to oral health?
A: The gut microbiome influences the immune system and inflammation throughout the body. An imbalanced gut microbiome can contribute to both oral and systemic diseases.
Q: Is there a link between oral bacteria and inflammatory bowel disease (IBD)?
A: Yes, studies suggest that certain oral bacteria found in periodontal disease may exacerbate IBD symptoms and inflammation in the gut.
Q: Can treating gum disease improve digestive health?
A: Potentially. By reducing oral inflammation and harmful bacteria, treating gum disease may help improve the balance of the gut microbiome and alleviate some digestive symptoms.
Q: What role does diet play in the connection between oral and gut health?
A: Diet significantly impacts both oral and gut health. A diet high in sugar and processed foods can promote harmful bacteria in both the mouth and gut, increasing the risk of disease.
Q: What are some preventative measures I can take to protect both my oral and digestive health?
A: Maintain good oral hygiene (brushing, flossing, regular dental checkups), eat a balanced diet rich in fiber and low in processed foods, manage stress, and avoid smoking.
Q: When should I consult a healthcare professional about oral and digestive health concerns?
A: If you experience persistent oral symptoms (bleeding gums, ulcers, dry mouth) along with digestive issues (abdominal pain, bloating, diarrhea, constipation), consult your dentist and/or a gastroenterologist for evaluation and treatment.