Diagnosing TMJ Disorders: What to Expect During Your Evaluation
Diagnosing TMJ Disorders !!! So, your jaw’s been acting up, huh? Maybe it’s clicking, popping, or just plain achy. You might even be getting earaches or headaches that seem to come out of nowhere. If any of this sounds familiar, you might be dealing with a Temporomandibular Joint Disorder, or TMJ disorder for short. Don’t sweat it! While TMJ can be a real pain in the… well, jaw, getting a diagnosis is the first step to feeling like yourself again.
What’s the Deal with TMJ Disorders?
TMJ disorders, or TMD, are a group of conditions that cause pain and dysfunction in the jaw joint and muscles that control jaw movement. Think of it as a glitch in the hinge that connects your jaw to your skull. This hinge, a.k.a. the temporomandibular joint, lets you talk, chew, and yawn. When it’s not working right, it can lead to a whole host of annoying and sometimes debilitating symptoms.
The TMJ Diagnosis Journey: What to Expect
Okay, so you’re ready to figure out what’s going on with your jaw. What can you expect when you go in for a TMJ evaluation? The diagnosis of TMD is based largely on history and physical examination findings. Here’s the lowdown:
The Heart-to-Heart (Medical History):
- First up, your doctor or dentist will want to get the full story. They’ll ask you a bunch of questions about your symptoms, like where the pain is, when it started, and what makes it better or worse. They’ll also want to know about any past treatments, related conditions, and your medical and dental history[1]. Be prepared to discuss:
- Pain Patterns: When does it hurt the most? Is it a constant ache or does it come and go?
- Triggers: What seems to set off the pain? Stress? Certain foods?
- Other Symptoms: Are you experiencing headaches, ear pain, or dizziness?
- Past Treatments: Have you tried anything already to relieve the pain?
- The Physical Exam: Getting Hands-On:
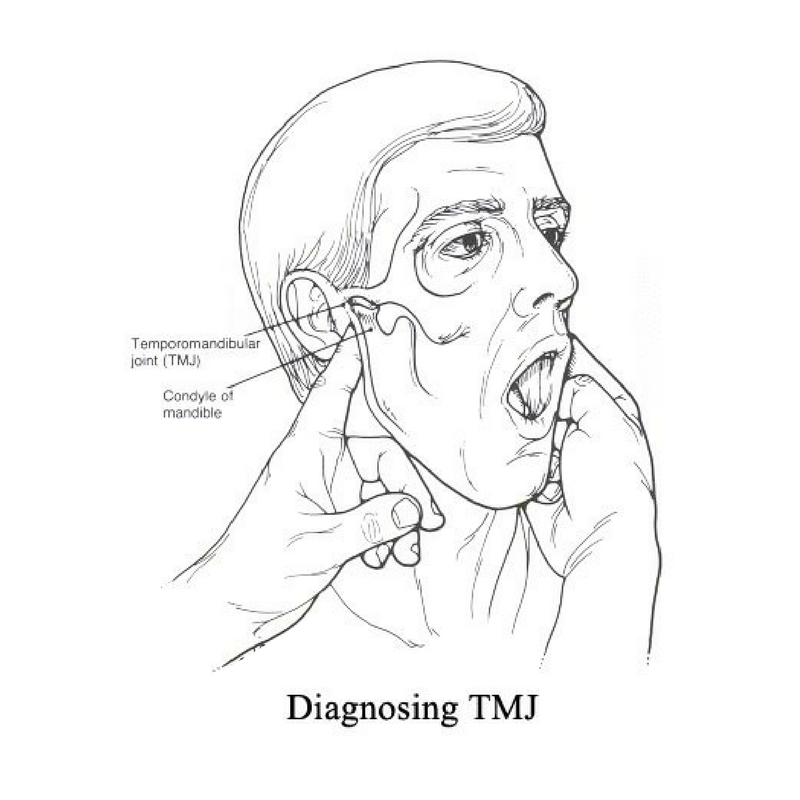
- Next, it’s time for a physical examination. Your dentist will check your head, neck, face, and jaw for any tenderness, and listen for any popping or clicking when you move your jaw[1][2]. They will also evaluate your bite to see how your teeth come together[1]. This part is crucial because it gives your dentist valuable insights into what’s causing your discomfort. Here’s what they’ll be looking at:
- Jaw Movement: How far can you open your mouth? Is it a smooth motion or is there any stiffness?
- Joint Sounds: Any clicks, pops, or grating noises when you open and close your mouth?
- Muscle Tenderness: Do you flinch when they press on certain spots around your jaw, head, or neck?
- Bite Evaluation: Checking for signs of teeth grinding or clenching.
The “Say Ahh” (Range of Motion Tests):
- Your dentist will also check the extent to which you can move your jaw in different directions[1][2]. This helps them understand the range of motion in your jaw and identify any restrictions or limitations[1]. Normally, the jaw opens about 45 to 50 mm; if the disk is deranged, it will open about ≤ 30 mm and the jaw will deflect to the affected side[3].
- The Palpation Examination:
- Your dentist will feel your jaw and surrounding areas to identify any points of discomfort or abnormalities[1][2]. This helps them pinpoint the source of your pain and determine the extent of the problem. Pain with joint palpation will be assessed[6].
- The Imaging Studies (If Needed):
- Sometimes, your dentist might want to get a better look inside your jaw joint[1]. That’s where imaging studies come in[1]. These aren’t always necessary, but they can be helpful in ruling out other problems or getting a clearer picture of what’s going on[1]. Common imaging techniques include:
- X-rays: To get a good look at your teeth and jaw[1][2].
- CT Scans: To show detailed images of the bones involved in the joint[2].
- MRIs: To show issues with the joint’s disk or surrounding soft tissue[2].
- TMJ Arthroscopy: In some cases, a minimally invasive procedure may be used for both diagnosis and treatment[2]. During TMJ arthroscopy, your healthcare professional inserts a small thin tube called a cannula into the joint space[2]. Then a small camera called an arthroscope is inserted to look at the area and help find a diagnosis[2].
Deciphering the Results and Plotting a Course of Action
So, you’ve been poked, prodded, and maybe even had some pictures taken of your jaw. Now what? Your dentist will analyze all the information gathered during the evaluation to figure out what’s causing your TMJ symptoms[1][4]. The correct indication of an imaging study should be based on the patient’s need for legal documentation, his/her individual complaints, and the identified clinical signs and symptoms obtained during history-taking and physical examination[4].
Once they’ve got a diagnosis, they’ll work with you to develop a treatment plan[4]. This might involve:
- Lifestyle Changes: Simple stuff like avoiding chewing gum, eating soft foods, and using ice packs can sometimes make a big difference.
- Medications: Pain relievers, muscle relaxants, or anti-inflammatory drugs can help manage pain and inflammation.
- Physical Therapy: Exercises to strengthen your jaw muscles and improve range of motion.
- Mouthguards: To prevent teeth grinding and clenching, especially at night.
- Other Treatments: In some cases, more advanced treatments like injections or even surgery might be necessary.
Easing Your Worries: What to Keep in Mind
Let’s be real, going to the dentist can be stressful, especially when you’re dealing with pain. But here’s the thing: getting a TMJ diagnosis is all about finding answers and getting you on the road to recovery. The TMD diagnostic process also relies on a psychosocial assessment of patients.
- Communication is Key: Don’t be afraid to ask questions and voice your concerns. The more your dentist knows about what you’re experiencing, the better they can help you.
- It’s Not Always a Quick Fix: TMJ treatment can take time and patience. Be prepared to try different approaches and work closely with your dentist to find what works best for you.
- You’re Not Alone: TMJ disorders are pretty common. There are tons of people out there who know exactly what you’re going through.
The Bottom Line in Diagnosing TMJ Disorders
Look, TMJ disorders can be a real drag. But with a proper diagnosis and treatment plan, you can get back to living your life without that constant jaw pain. So, if you think you might have TMJ, don’t wait. Get yourself checked out and start your journey to a happier, healthier jaw!
FAQs
1. What are TMJ disorders (TMD)?
TMD refers to a group of conditions causing pain and dysfunction in the jaw joint and muscles controlling jaw movement.
2. What symptoms suggest I might need a TMJ evaluation?
Common symptoms include jaw pain, clicking or popping in the jaw, difficulty opening or closing your mouth, headaches, earaches, and tenderness in the jaw muscles.
3. What will happen during my first TMJ evaluation?
The evaluation typically involves a review of your medical history, a physical examination of your head, neck, face, and jaw, and an assessment of your jaw’s range of motion.
4. What kind of questions will the doctor ask about my pain?
Expect questions about the location, intensity, and timing of your pain, as well as any triggers or factors that worsen or relieve it.
5. Will the dentist physically examine my jaw?
Yes, the dentist will feel your jaw and surrounding areas for tenderness, listen for joint sounds, and assess your bite.
6. Are imaging tests always needed for a TMJ diagnosis?
No, imaging tests like X-rays, CT scans, or MRIs aren’t always necessary. They are used if the dentist needs a clearer picture or to rule out other problems.
7. What do range of motion tests involve?
The dentist will check how far you can move your jaw in different directions to identify any limitations or restrictions.
8. How is a TMJ diagnosis made?
Diagnosis is primarily based on your medical history and the findings of the physical examination.
9. What kind of treatments might be recommended after a TMJ diagnosis?
Treatment options range from lifestyle changes and medications to physical therapy, mouthguards, and, in some cases, more advanced interventions like injections or surgery.
10. How long does TMJ treatment typically take?
: TMJ treatment can take time and patience, and it may involve trying different approaches to find what works best for you.







